Differentiating Headaches and Four Different Types of Migraines:
Connecting Students’ Sensory and Neurological Functioning with School Learning, Socialization, and Disabilities (Part II)
Listen to a summary and analysis of this Blog on the Improving Education Today: The Deep Dive podcast on Spotify.
Hosted by popular AI Educators Angela Jones and Davey Johnson, they provide enlightening perspectives on the implications of this Blog for all of Education.
[CLICK HERE to Listen to this Popular Podcast]
(Follow this bi-monthly Podcast to receive automatic e-mail notices with each NEW episode!)
Dear Colleagues,
Introduction
Just one of my professional “hats” is as an Expert Witness on Federal, State, and special education/disability rights due process cases involving children and adolescents.
In fact, I have been involved in over 25 federal courts cases (some settled before they got to trial), written nearly 20 expert reports, been deposed or testified in due process hearings 30 or more times, and worked directly with the staff in two State Attorney Generals’ Offices.
While sometimes tense and confrontative, I enjoy the challenge. And my cases—combined—have involved:
- IDEA and Special Education Procedures
- School Psychology Assessment/Intervention Disputes
- Psychological Misdiagnoses and Mental Health Services
- 504 Accommodations and Disability Rights
- Title IX Sexual Harassment Violations
- Disproportionality and Racial Discrimination/Equity
- Emotionally Disturbed and Students on the Autism Spectrum
- Seclusion and Restraints
- Educational Malpractice, School Safety and Violence
- Social-Emotional Learning and Positive Behavioral Supports
- Multi-Tiered Systems of Support
- Bullying and Physical Aggression
- Discipline and Corporal Punishment
- IEP Disputes and Due Process Hearings
- FAPE and LRE
- Learning Disabilities and ADHD
- Stress and Trauma
_ _ _ _ _
Many times, as an Expert Witness, I am asked to evaluate the social and developmental history and status of the students involved in my cases—especially how their health, mental health, and cognitive status relates to their academic and/or social, emotional, or behavioral learning, interactions, and success.
Broadly speaking, students’ “health” involves their physical, sensory, physiological, neurological, hormonal, biochemical, and related functioning.
And my knowledge of these biological systems is especially important when, for example, my court cases involve motor vehicle accidents, emergency room errors, students with concussions from physical assaults, or students with neurological anomalies, dyslexia, or multiple disabilities.
And yet, an ongoing issue in court is whether the presiding Judge will allow me to testify as an Expert in the areas above.
As I said at the very beginning of Part I of this multi-part Blog Series, “I am not a doctor.”
But from a legal perspective, I am not in court to diagnose the medical conditions of a child or adolescent. That’s what doctors and other medical experts do.
Instead, as above, I am in court—and fully able—to discuss the academic/learning and social, emotional, and behavioral implications of selected biologically-based conditions.
In fact, I am typically the only expert able to do this.
Indeed, I learned this early on in my career when I asked a pediatric neurologist how a student’s traumatic brain injury was going to impact his learning and social interactions.
The neurologist. . . and many others since. . . looked at me and replied, “I don’t know. That’s your job as the school psychologist.”
_ _ _ _ _
A Blog Series Reintroduction
Part I of this Blog Series discussed the wide assortment of disabilities that qualify students for services either under Section 504 of the Rehabilitation Act of 1973 or the Individuals with Disabilities Act (IDEA, 2004), respectfully.
Connecting Students’ Sensory and Neurological Functioning with School Learning, Socialization, and Disabilities:A Primer on Vision, Hearing, and Respiratory/Nasal Functioning (Part I)
_ _ _ _ _
In Part I, we noted that virtually every one of the 504 disabilities discussed—and virtually every one of the thirteen disabilities in IDEA—has an important relationship to the biological, physical or physiological, biochemical, or neuropsychological functioning of the students involved.
Moreover, we stressed that the different multi-disciplinary experts on every school’s 504, IDEA, or MTSS (Multi-Tiered System of Supports) team need to understand these biological-disability connections. . . from a curriculum, instruction, and learning perspective, as well as from an assessment, accommodation, and intervention perspective.
Finally, we emphasized that this expertise helps (a) create bridges between medical and educational professionals; (b) dismantles misconceptions that students with disabilities are simply choosing to be unsuccessful; (c) defuses beliefs that poor parenting, supervision, or motivation is to blame; and (d) promotes more empathetic and compassionate interactions by peers, staff, and administrators.
_ _ _ _ _
This first Blog in this multi-part Series connected students’ sensory and neurological functioning in the areas of vision, hearing, and respiratory/nasal functioning with their school learning, socialization, and disabilities.
This Blog—Part II will address the same sensory and neurological connections relative to students’ headaches and migraines.
Headaches vs. Migraines: What’s the Difference?
Most people have experienced a headache at some point in their lives, and yet not all “head pains” are created equal. While “having a headache” is often used as a catch-all term, a migraine represents a distinct neurological condition with unique characteristics, root causes, and treatment approaches.
Headaches are typically felt as pain or pressure in the head or neck region, and they range from mild to severe. They can last from 30 minutes to several hours. And they occur due to a variety of causes—including tension, dehydration, sinus issues, or underlying medical conditions.
Headaches are typically categorized into “primary headaches,” which occur independently (like tension headaches), and “secondary headaches,” which result from other conditions (such as infections). Most headaches respond well to over-the-counter pain relievers, and rarely interfere with an individual’s daily activities.
Migraines, however, are more complex.
They're characterized by intense, throbbing pain that is often concentrated on one side of the head. What sets migraines apart is that they are frequently accompanied by additional symptoms like nausea, vomiting, and extreme sensitivity to light and sound. Many migraine sufferers also experience "aura" symptoms—visual disturbances such as flashing lights or blind spots—that precede the headache phase.
Migraines also significantly differ in their duration. While typical headaches resolve relatively quickly, migraines can persist for days, often forcing sufferers to retreat to dark, quiet rooms until the episode passes. Perhaps most tellingly, migraines substantially impact the quality of a person’s life, with many people unable to function normally during an attack.
Migraines often require specialized medication and comprehensive management strategies that are developed with healthcare providers. While all migraines are headaches, not all headaches are migraines.
The Silent Storm: How Migraines Disrupt Student Learning and Participation
For students who suffer from migraines, these neurological events can dramatically impact every aspect of their educational experience, creating obstacles that many teachers and peers may not fully understand.
Some of the most-significant ways that migraines interfere with learning, school interactions, and classroom participation are listed below.
Cognitive Disruption During Attacks
When a migraine strikes, it doesn't just bring pain—it creates a cognitive fog that makes learning nearly impossible.
Students experiencing migraines often experience:
- Difficulty focusing on lectures or reading materials
- Impaired ability to process and retain new information
- Challenges with critical thinking and problem-solving
- Decreased speed in completing assignments or tests
These cognitive effects can persist even after the pain subsides, creating what many migraine sufferers call a "hangover" effect that can last for days.
_ _ _ _ _
Attendance and Consistency Issues
The unpredictable nature of migraines presents significant challenges to regular school attendance.
Students with chronic migraines may:
- Miss full or partial school days during attacks
- Struggle to maintain continuity in their learning
- Fall behind on sequential material in subjects like math or language
- Miss important group work, presentations, or hands-on activities
This inconsistent attendance creates gaps that become increasingly difficult to bridge, especially in fast-paced academic environments.
_ _ _ _ _
Classroom Participation Barriers
Even when physically present, migraine sufferers often cannot fully engage in classroom activities.
Common participation obstacles include:
- Sensitivity to classroom lighting (especially fluorescent lights)
- Difficulty with noise levels during collaborative work
- Challenges with screen time requirements
- Hesitancy to speak up due to pain or medication side effects
These barriers can lead to misperceptions about a student's interest, preparation, or intellectual capabilities when the reality is simply that they're navigating their education through a neurological challenge.
_ _ _ _ _
Social and Emotional Impact
The social dimensions of living with migraines in an educational setting shouldn't be overlooked.
Students may experience:
- Isolation from peers who don't understand their condition
- Anxiety about potential migraine triggers in school environments
- Frustration when having to repeatedly explain their invisible disability
- Stress about making up missed work or assessments
These social-emotional factors create additional layers of difficulty beyond the direct neurological effects of migraines themselves.
_ _ _ _ _
Academic Performance Consequences
The combined impact of these challenges often affects academic performance in ways that don't reflect a student's true abilities or effort.
Migraine-affected students might:
- Perform inconsistently across assignments or exams
- Struggle with timed assessments during prodrome or postdrome phases
- Face challenges with memory-intensive tasks during migraine cycles
- Experience decreased performance during high-stress periods that trigger attacks
_ _ _ _ _
Understanding these impacts is crucial for educators and institutions seeking to provide appropriate accommodations and support for students navigating their education while managing migraines.
The Typical Neurological, Limbic, and Biochemical Pathways of Migraines
Impacting the quality of life for millions of people worldwide, migraines involve complex neurological conditions with distinct characteristics, underlying mechanisms, and sensory or other origins.
Relative to the latter, we will later discuss four types of migraines: Retinal migraines, Vestibular migraines, Concussion-related migraines, and Stress or Post-Traumatic Stress Syndrome (PTSD) migraines.
At the same time, these different types of migraines utilize many common neurological, limbic, and biochemical structures and pathways in—especially—the brain.
While the administrators and related service professionals on a school’s MTSS Team are not qualified to differentially and medically diagnose different migraines, it is important that they understand their common and distinct characteristics so that they can effectively:
- Communicate with the students involved, their parents, and—with permission—anyone diagnosing or treating an individual student; and
- Ensure that school-specific accommodations and/or interventions are accurate, well-designed, and implemented with integrity.
The common migraine-related systems and pathways are described below. This will be followed by separate sections discussing the four different types of migraines referenced above.
_ _ _ _ _
Brain Structures and Chemical Systems Common to Migraines
As noted, migraines are complex neurological events that involve multiple brain structures and chemical systems. Here is a quick overview of the key brain regions and neurotransmitters that contribute to migraine pathophysiology (see also Figure 1).
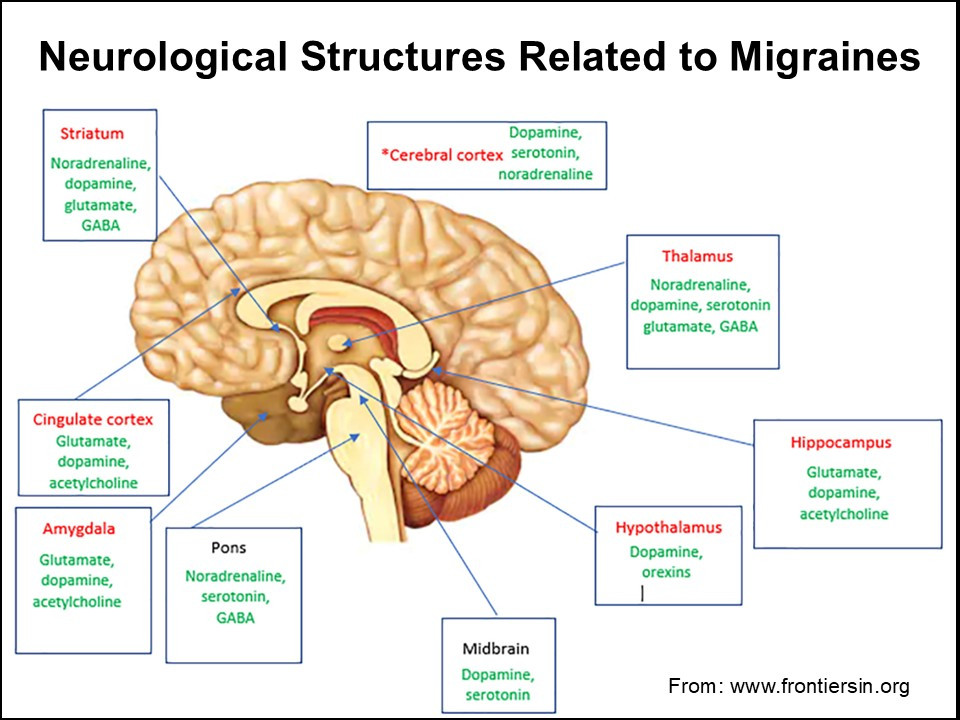
Amygdala. The amygdala is an almond-shaped cluster of nuclei located deep within the temporal lobes of the brain. As a central component of the limbic system, it serves as the brain's emotional processing center and alarm system. Among its primary functions are the following:
- Emotional Processing. Evaluates emotional significance of stimuli, particularly fear, threat, and danger
- Fear Conditioning. Forms associations between neutral stimuli and threatening experiences
- Stress Response. Activates physiological reactions to threatening situations
- Social Cognition. Processes facial expressions and social cues related to emotion
- Emotional Memory. Enhances encoding and storage of emotionally charged experiences
_ _ _ _ _
Hippocampus. The hippocampus is a seahorse-shaped structure nestled in the medial temporal lobe. It plays a crucial role in learning and memory formation and acts as a cognitive map-maker for navigating our physical and mental worlds. Among its primary functions are the following:
- Memory Formation. Critical for converting short-term memories into long-term memories
- Spatial Navigation. Creates cognitive maps of environments and supports spatial awareness
- Contextual Learning. Binds together various elements of an experience
- Stress Regulation. Provides negative feedback to the HPA axis during stress responses
- Neurogenesis. One of few brain regions where new neurons continue to form throughout life
_ _ _ _ _
Prefrontal Cortex. The prefrontal cortex is the most evolved region of the frontal lobe, located at the very front of the brain. It serves as the brain's executive center, coordinating thoughts and actions in accordance with internal goals and external demands. Among its primary functions are the following:
- Executive Functions. Manages planning, decision-making, and problem-solving
- Impulse Control. Inhibits inappropriate behaviors and emotional responses
- Working Memory. Temporarily holds and manipulates information
- Social Behavior. Guides appropriate social interactions and understanding social norms
- Cognitive Flexibility. Adapts thinking and behavior to changing situations
- Attention Regulation. Focuses mental resources on relevant stimuli
_ _ _ _ _
Hypothalamus. The hypothalamus is a small but critical structure located below the thalamus, serving as the brain's primary link between the nervous and endocrine systems. It functions as the body's homeostatic command center, ensuring physiological systems remain in balance. Among its primary functions are the following:
- Homeostasis. Regulates body temperature, hunger, thirst, fatigue, and sleep
- Endocrine Control. Connects the nervous system to the endocrine system via the pituitary gland
- Autonomic Nervous System Regulation. Controls involuntary functions like heart rate and digestion
- Circadian Rhythms. Helps establish daily physiological cycles
- Emotional Responses. Contributes to feelings of pleasure, anger, and fear through connections with the limbic system
_ _ _ _ _
Neurotransmitters. Neurotransmitters are chemical messengers that transmit signals across synapses from one neuron to another. These specialized molecules serve as the language of the nervous system, enabling communication between brain cells and influencing nearly every function of body and mind. Some of the most important groups of neurotransmitters here are:
Excitatory Neurotransmitters
- Glutamate. Primary excitatory neurotransmitter; critical for learning, memory, and synaptic plasticity
_ _ _ _ _
Inhibitory Neurotransmitters
- GABA (Gamma-Aminobutyric Acid). Primary inhibitory neurotransmitter; regulates anxiety, muscle tension, and prevents overexcitation
_ _ _ _ _
Neuromodulators
- Dopamine. Regulates motivation, reward, pleasure, motor control, and executive functions
- Serotonin. Modulates mood, appetite, sleep, memory, learning, and social behavior
- Norepinephrine. Involved in arousal, attention, stress response, and vigilance
- Acetylcholine. Controls muscle activation, attention, arousal, and memory formation
- Endorphins. Natural painkillers that produce feelings of well-being and pleasure
_ _ _ _ _
The Neurological Basis of Migraines
With the foundational information above, here are the how the key brain regions and neurotransmitters contribute to migraine pathophysiology.
Amygdala. The amygdala plays a significant role in migraines by:
- Amplifying the perception of pain during migraine attacks
- Contributing to stress-induced migraines through its hyperactivity
- Mediating anxiety and emotional responses that often accompany migraines
- Sensitizing the individual to recurring pain, potentially making future migraines more likely
_ _ _ _ _
Hippocampus. The hippocampus affects migraines through:
- Creating "pain memories" that may lower the threshold for future migraine attacks
- Reducing the volume of this brain structure, contributing to difficulties in distinguishing between past and present threats, leading to the intrusive memories and flashbacks
- Mediating stress responses via the hypothalamus, pituitary, adrenal (HPA) axis, influencing migraine susceptibility
- Contributing to spatial and contextual associations with migraine triggers
_ _ _ _ _
Prefrontal Cortex. The prefrontal cortex impacts migraines by:
- Exhibiting reduced activity during migraine attacks, impairing cognitive functioning
- Participating in pain modulation and inhibitory control
- Showing altered connectivity patterns in migraine patients
- Mediating attention to pain signals and emotional responses to pain
_ _ _ _ _
Hypothalamus. The hypothalamus contributes to migraines through:
- Initiating the prodromal phase with early warning symptoms
- Controlling sleep-wake cycles, disruptions of which can trigger migraines
- Regulating appetite and food cravings associated with migraine phases
- Coordinating autonomic responses like nausea and sensitivity to light and sound
_ _ _ _ _
Neurotransmitters. The neurotransmitters that are central to migraine pathophysiology are:
- Serotonin (5-HT). Changes in serotonin levels can affect blood vessel diameter and pain signaling.
- Calcitonin Gene-Related Peptide (CGRP). This neuropeptide is released during migraine attacks, causing blood vessel dilation and neurogenic inflammation.
- Glutamate. Excessive glutamate activity contributes to cortical spreading depression (CSD; a wave of neural excitation followed by inhibition that is believed to underlie migraine aura), and can lead to neuronal hyperexcitability, contributing to migraine symptoms.
- GABA. Reduced activity of this inhibitory neurotransmitter may lower the threshold for migraine triggers and contribute to central sensitization.
- Dopamine. Implicated in prodromal and accompanying symptoms like nausea, yawning, and food cravings.
- Norepinephrine. Involved in pain modulation and stress responses that can influence migraine onset and severity.
_ _ _ _ _
Putting all of this together, here is how a migraine typically develops and progresses in the brain:
Prodrome Phase (1 to 2 days before headache)
- The brain begins experiencing subtle neurochemical changes
- Hypothalamus activation leads to early warning symptoms
- Altered serotonin and dopamine levels affect mood and energy
- Many experience food cravings, mood changes, or fatigue
_ _ _ _ _
Aura Phase (occurs in ~25% of migraine patients)
- Cortical spreading depression (CSD) occurs - a wave of electrical activity followed by inhibition that moves across the cerebral cortex
- Visual cortex involvement produces visual disturbances (flashing lights, zigzag lines)
- Can affect other cortical areas causing sensory, language, or motor symptoms
- Typically lasts 20 to 60 minutes before the headache begins
_ _ _ _ _
Headache Phase
- Trigeminal nerve activation leads to release of inflammatory neuropeptides
- Blood vessels dilate and become inflamed (neurogenic inflammation)
- Pain signals travel through the trigeminal nerve to the thalamus and cortex
- Sensitization of pain pathways occurs, making normal stimuli painful
- Brainstem activation contributes to associated symptoms like nausea
- Pain typically builds over 1-2 hours, peaks, and can last 4 to 72 hours
_ _ _ _ _
Postdrome Phase
- Brain returns to baseline but remains vulnerable
- Neurotransmitter depletion leads to fatigue and cognitive difficulties
- Blood flow patterns normalize gradually
- Patients often experience "brain fog," mild headache, or fatigue
- Can last 1 to 2 days after the headache resolves
Now, let's explore specific migraine types and their unique characteristics.
Differentiating Across Ocular/Retinal, Vestibular, Concussion-related, and Stress or Post-Traumatic Stress Syndrome Migraines
This section will compare and especially contrast the differences across retinal, vestibular, concussion-related, and stress or post-traumatic stress syndrome migraines. For each type, we will provide the following information relative to its:
- Clinical Presentation
- Neurobiological Mechanisms
- Diagnostic Considerations
- Management Approaches
While it is critical to understand each respective migraine’s root causes, manifestations, and courses of treatment, a differential diagnosis still must be rendered by a medical professional.
At the same time, different medical specialists (e.g., Ear, Nose, and Throat; Neurologists, Ophthalmologists) are not necessarily expert in all of these different types of migraine. Moreover, diagnoses of stress or Post-Traumatic Stress Syndrome (PTSD) migraines clearly should involve psychiatrists, neuropsychologists, or psychologists with specialized stress/PTSD training.
Critically, when interacting with students exhibiting migraines in school settings, MTSS Team members should understand the information below. . . at the very least, so that they can ask informed questions when conferring with parents and—with permission—medical professionals.
For school psychologists and clinical social workers trained in stress and PTSD, this information is especially essential as they will need to dismiss the other types of migraines before accurately confirming a migraine that is caused by stress or PTSD.
_ _ _ _ _
Ocular/Retinal Migraines: When Vision Takes Center Stage
Ocular migraines (sometimes called retinal migraines) represent a distinct migraine variant that is characterized primarily by visual disturbances with or without headache pain.
Clinical Presentation
- Visual Symptoms. Temporary vision loss or blindness in one eye (monocular), flickering lights, blind spots, or zigzag patterns
- Temporal Profile. Episodes typically lasting 5 to 30 minutes, rarely exceeding one hour
- Headache Relationship. May occur before, during, or after headache phase; sometimes occurs without headache
- Triggers. Similar to common migraines, but often include visual stimuli (bright lights, screen time, glare)
- Distinguishing Feature. True ocular migraines affect only one eye, which can be confirmed by covering each eye separately during an episode
_ _ _ _ _
Neurobiological Mechanisms
Ocular migraines involve several specific neural pathways:
- Retinal Blood Vessel Dynamics. Transient vasoconstriction of the retinal or ciliary blood vessels leads to hypoperfusion—a decreased blood flow to and oxygenation of the retina
- Visual Cortex Hyperexcitability. Abnormal excitation patterns in primary and secondary visual cortices
- Ophthalmic Trigeminal Activation. The ophthalmic (V1) division of the trigeminal nerve becomes sensitized
- Neurovascular Coupling Disruption. Impaired coordination between neuronal activity and blood flow in visual processing areas
_ _ _ _ _
Diagnostic Considerations
Diagnosis requires ruling out other serious conditions that can cause similar symptoms such as Transient ischemic attacks (TIAs), Amaurosis fugax, Retinal detachment, Optic neuritis.
_ _ _ _ _
Management Approaches
Ocular migraine management focuses on:
- Trigger Identification. Detailed visual trigger monitoring (blue light exposure, screen time patterns)
- Preventive Medications. Calcium channel blockers (like verapamil) have shown specific efficacy for ocular variants
- Visual Rehabilitation. Specialized vision therapy and visual ergonomic adjustments
- Neuromodulation. Targeted approaches to regulate visual cortex excitability
_ _ _ _ _
Retinal Migraines: When the Retina Rebels
While sometimes used interchangeably with ocular migraines, retinal migraines specifically refer to migraine variants where reduced blood flow to the retina causes temporary vision disturbances.
Clinical Presentation
- Strictly Monocular Symptoms. Visual disturbances always confined to one eye
- Visual Manifestations. Scintillations (flashing lights), scotoma (partial vision loss), or complete but temporary blindness
- Duration. Brief episodes, usually 5-20 minutes, seldom exceeding 60 minutes
- Associated Symptoms. May be accompanied by photophobia and nausea
- Recurrence Pattern. Typically affects the same eye during repeated episodes
_ _ _ _ _
Neurobiological Mechanisms
Retinal migraines distinctly involve:
- Retinal Vasospasm. Pronounced constriction of blood vessels specifically affecting the retina
- Retinal Spreading Depression. A wave of depolarization similar to cortical spreading depression but occurring in retinal tissue
- Hypoperfusion Patterns. Distinct patterns of reduced blood flow to retinal cells affecting specific visual fields
- Neurotransmitter Involvement. Serotonin and endothelin play key roles in retinal vessel tone regulation
- Glutamate Excitotoxicity. Excessive activation of glutamate receptors in retinal neurons causing temporary dysfunction
_ _ _ _ _
Diagnostic Approach
Diagnosis should include: a thorough ophthalmologic examination, visual field testing during and between episodes (if possible), fluorescein angiography to evaluate retinal blood flow, and optical coherence tomography (OCT) to assess retinal structure.
_ _ _ _ _
Management Considerations
Specific approaches for retinal migraines include:
- Vasodilators. Medications like calcium channel blockers and magnesium supplementation to prevent vasospasm
- Neuroprotective Strategies. Agents that may protect retinal cells during hypoxic episodes
- Thrombosis Prevention. Low-dose aspirin may be considered in some cases
- Specialized Monitoring. Regular ophthalmologic follow-up to ensure no progressive vascular pathology
_ _ _ _ _
Vestibular Migraines: When Balance Is Disrupted
Vestibular migraines represent a fascinating intersection of headache and balance disorders, often misdiagnosed as separate conditions.
Clinical Presentation
- Vestibular Symptoms. Vertigo (true spinning sensation), disequilibrium, motion sensitivity, spatial disorientation
- Temporal Pattern. Vestibular symptoms lasting minutes to days, often outlasting headache phase
- Headache Relationship. May occur with simultaneous headache, but approximately 30% of episodes occur without headache
- Sensory Sensitivity. Pronounced sensitivity to motion, visual stimuli, and position changes
- Cognitive Impact. "Brain fog," difficulty concentrating, and spatial disorientation
- Autonomic Features. Nausea, vomiting, sweating, and pallor are common
_ _ _ _ _
Neurobiological Mechanisms
Vestibular migraines involve several specific neural pathways:
- Vestibular Nuclei Sensitization. Persistent heightened activity in brainstem vestibular nuclei
- Reciprocal Connections. Abnormal signaling between vestibular nuclei and trigeminal nerve nuclei
- Vestibulocerebellar Circuit Dysfunction. Altered processing in cerebellar pathways that modulate vestibular input
- Thalamocortical Dysregulation. Disrupted sensory processing in thalamic vestibular regions projecting to cortex
- Inner Ear Involvement. Functional changes in semicircular canals and otolith organs without structural damage
- Neurotransmitter Profile. Unique pattern of GABA, glutamate, and serotonin dysregulation in vestibular pathways
_ _ _ _ _
Diagnostic Approach
Diagnosis relies on: International Headache Society criteria for vestibular migraine, Videonystagmography (VNG) testing, Computerized dynamic posturography, Vestibular evoked myogenic potentials (VEMP), and Rotary chair testing to assess vestibular function
_ _ _ _ _
Management Considerations
Vestibular migraine management requires a specialized approach:
- Vestibular Rehabilitation Therapy. Customized exercises to improve vestibular adaptation and compensation
- Migraine Preventives. Particular efficacy seen with topiramate and amitriptyline for vestibular variants
- Vestibular Suppressants. Judicious use of medications like meclizine during acute episodes
- Lifestyle Modifications. Specific strategies to minimize visual-vestibular mismatch
- Balance Training. Proprioceptive exercises to improve balance system integration
- Neuromodulation. Emerging evidence for vestibular nerve stimulation techniques
_ _ _ _ _
Concussion-Related Migraines: The Post-Traumatic Cascade
Traumatic brain injuries (TBIs) can trigger a distinctive form of post-traumatic migraine, which may persist long after the initial injury has resolved.
Clinical Presentation
- Temporal Relationship. Headaches developing within 7 days of head trauma or after regaining consciousness
- Pain Characteristics. Often described as pulsating or pressure-like, frequently bilateral
- Sensory Hypersensitivity. Pronounced photophobia, phonophobia, and osmophobia
- Cognitive Symptoms. Impaired concentration, memory problems, slower processing speed
- Emotional Components. Irritability, anxiety, and emotional lability
- Sleep Disturbances. Insomnia, hypersomnia, or disrupted sleep patterns
- Duration. May persist for months or years post-injury
_ _ _ _ _
Neurobiological Mechanisms
Concussion-related migraines involve a complex cascade of events:
- Diffuse Axonal Injury. Microscopic damage to white matter tracts disrupting normal neural communication
- Neurometabolic Cascade. Initial hypermetabolic state followed by prolonged hypometabolism
- Blood-Brain Barrier Disruption. Increased permeability allowing inflammatory mediators to enter brain tissue
- Glial Activation. Prolonged microglial and astrocytic responses contributing to neuroinflammation
- Neurotransmitter Dysregulation. Excitatory-inhibitory imbalance, particularly affecting glutamate and GABA
- Altered Cerebral Blood Flow. Disrupted autoregulation and perfusion patterns
- Mitochondrial Dysfunction. Impaired energy production in neurons leading to oxidative stress
- Thalamic Sensitization. Central pain processing changes in thalamic nuclei
_ _ _ _ _
Diagnostic Considerations
Thorough assessment includes: Detailed concussion history and symptom timeline, Neurocognitive testing to quantify cognitive impacts, Neuroimaging (functional MRI may reveal changes not visible on structural scans), Balance and vestibular assessment, and Sleep evaluations.
_ _ _ _ _
Management Approaches
Post-traumatic migraine management requires a multifaceted approach:
- Neuroprotective Strategies. Early interventions to minimize secondary injury
- Controlled Cognitive Exertion. Carefully titrated mental activity resumption
- Neuromodulation. Transcranial magnetic stimulation shows promise for post-traumatic patterns
- Cognitive Rehabilitation. Targeted approaches for specific cognitive deficits
- Pharmacological Management. Consideration of migraine preventives with neuroprotective properties
- Autonomic Regulation. Heart rate variability biofeedback and related approaches
- Sleep Optimization. Aggressive management of post-traumatic sleep disturbances
- Vestibular Therapy. When concurrent vestibular symptoms are present
_ _ _ _ _
PTSD-Related Migraines: The Mind-Body Connection
The relationship between post-traumatic stress disorder (PTSD) and migraines represents one of the most complex interactions between psychological trauma and neurobiological responses.
Clinical Presentation
- Trigger Sensitivity. Headaches triggered by trauma reminders or stress
- Hyperarousal Features. Exaggerated startle response, hypervigilance, and heightened sensory sensitivity during migraine episodes
- Autonomic Activation. Pronounced sympathetic nervous system symptoms (rapid heartbeat, sweating, trembling)
- Dissociative Elements. Some patients report dissociative symptoms during migraine attacks
- Comorbidities. High rates of anxiety, depression, and sleep disorders
- Chronification Risk. Higher likelihood of developing chronic daily headache
- Treatment Resistance. Often less responsive to standard migraine treatments alone
_ _ _ _ _
Neurobiological Mechanisms
PTSD-related migraines involve specific neural circuits:
- Amygdala Hyperreactivity. Exaggerated and persistent activation of fear-processing circuits
- Prefrontal Cortex Hypoactivation. Reduced top-down control over limbic structures
- HPA Axis Dysregulation. Abnormal cortisol patterns affecting stress response and pain perception
- Periaqueductal Gray (PAG) Dysfunction. Impaired descending pain modulation
- Autonomic Nervous System Imbalance. Predominantly sympathetic ("fight-or-flight") activation with inadequate parasympathetic recovery
- Inflammatory Profile. Distinctive pattern of elevated pro-inflammatory cytokines
- Neurotransmitter Alterations. Dysregulation of serotonin, norepinephrine, and GABA systems
- Epigenetic Changes. Trauma-induced epigenetic modifications affecting genes involved in stress response and pain processing
_ _ _ _ _
Diagnostic Approach
Assessment should include: Trauma history and PTSD screening, Headache characteristics and relationship to trauma triggers, Autonomic symptom assessment, Sleep evaluation, and Comorbid mood disorder assessment.
_ _ _ _ _
Management Considerations
Effective management requires addressing both PTSD and migraine mechanisms:
- Trauma-Focused Therapy. Evidence-based approaches like EMDR or trauma-focused CBT
- Autonomic Regulation. Heart rate variability biofeedback and related approaches
- Pharmacological Considerations. Medications addressing both conditions (e.g., SNRIs like venlafaxine)
- Mindfulness-Based Interventions. Practices specifically adapted for trauma and pain
- Sleep Restoration. Trauma-informed approach to sleep improvement
- Body-Based Approaches. Somatic experiencing and other body-centered therapies
- Neuromodulation. Emerging evidence for techniques targeting both PTSD and migraine circuits
_ _ _ _ _
Integrating Specific Student Treatment Approaches
As shown above, it is important to understand that the effective management of these specialized types of migraines require a comprehensive approach that addresses their unique neurological, limbic, and biochemical pathways.
To summarize, an integrative treatment framework includes:
Personalized Assessment
- Detailed migraine phenotyping to identify specific variant
- Trigger identification and pattern recognition
- Comprehensive neurological evaluation
- Advanced neuroimaging when indicated
- Vestibular and visual function testing
- Sleep and autonomic function assessment
_ _ _ _ _
Neurological Regulation
- Targeted neurofeedback protocols specific to migraine type
- Transcranial magnetic stimulation with montages specific to migraine variant
- Vagus nerve stimulation to modulate autonomic responses
- Visual rehabilitation for ocular/retinal variants
- Vestibular therapy for vestibular variants
_ _ _ _ _
Limbic Retraining
- Stress reduction techniques focusing on amygdala regulation
- Mindfulness practices to improve emotional processing
- Trauma-informed approaches for PTSD-related migraines
- Cognitive-behavioral strategies targeted to specific migraine types
- Interoceptive awareness training
_ _ _ _ _
Biochemical Optimization
- Nutritional interventions targeting inflammatory pathways
- Targeted supplementation for neurotransmitter support
- Hormonal balance assessment and support
- Oxidative stress reduction
- Mitochondrial support strategies
_ _ _ _ _ _ _ _ _ _
Summary
This is the second Blog of a multi-part Blog Series focusing broadly on three clusters of biologically-based conditions and their impact on students’ academic and/or social, emotional, or behavioral learning, interactions, and success. The first Blog addressed Vision, Hearing, and Respiratory/Nasal functioning, while this Blog discussed headaches and migraines.
In this second Blog, we initially distinguished between headaches and migraines, and described how migraines affect students academically and socially in school.
We then discussed four types of migraines: Ocular/Retinal, Vestibular, Concussion-related, and Stress or Post-Traumatic Stress Syndrome migraines. This was done by addressing their (a) common neurological, limbic, and biochemical structures and pathways; and (b) their distinct clinical presentations, neurobiological mechanisms, diagnostic considerations, and management approaches.
Migraines involve complex neurological conditions with distinct characteristics, underlying mechanisms, and sensory or other origins. While it was emphasized that the differential diagnoses of these migraines must be rendered by medical professionals, when interacting with students exhibiting headaches or migraines in school settings, MTSS (Multi-Tiered System of Supports) Team members should still understand their clinical similarities and differences. . . at the very least, so that they can ask informed questions when conferring with parents and—with permission—medical professionals.
Virtually every disability addressed by Section 504 of the Rehabilitation Act of 1973 and the Individuals with Disabilities Education Act of 2004 has an important relationship to the biological, physical or physiological, biochemical, or neuropsychological functioning of the students involved. MTSS team members need to understand the biological-disability connections discussed thus far in this Series. . . from a curriculum, instruction, and learning perspective, as well as from an assessment, accommodation, and intervention perspective.
_ _ _ _ _
The “Improving Education Today” Podcast: A New Professional Development Resource Complementing this Blog
This past January, we announced a new partnership and resource for you.
The partnership is with popular AI Educators, Davey Johnson and Angela Jones. . . and the resource is their Podcast:
Improving Education Today: The Deep Dive
For each published bimonthly Blog, Davey and Angela summarize and analyze the Blog in their free-wheeling and “no-holds-barred” Podcast. . . addressing the topic’s importance to “education today,” and discussing their recommendations on how to apply the information so that all students, staff, and schools benefit.
You can find the Podcast that accompanies this Blog message at the following link:
Improving Education Today: The Deep Dive | Podcast on Spotify
Davey and Angela have also created a Podcast Archive consisting of all of this year’s Blog (Volume 3), as well as those from 2024 (Volume 2), and 2023 (Volume 1).
The Podcasts are posted on Spotify, and you can “Follow” the Podcast Series so that you will be automatically notified whenever a new Podcast is posted.
Many districts and schools are using the Podcasts in their Leadership Teams and/or PLCs to keep everyone abreast of new issues and research in education, and to stimulate important discussions and decisions regarding the best ways to enhance student, staff, and school outcomes.
If you would like to follow a Podcast up with a free one-hour consultation with me, just contact me and we will get it on our schedules.
I hope to hear from you soon.
Best,
Howie
[To listen to a synopsis and analysis of this Blog on the “Improving Education Today: The Deep Dive” podcast on Spotify: CLICK HERE]